NP, PA or MD? Deciphering Your Healthcare Career Choices
Public Opinions about Medical Careers
It’s a familiar scenario. If your experiences have been anything like mine, articulating your dream of becoming a physician can lead to a flurry of questions and opinions. I’ve received comments ranging from “You should be a Nurse Practitioner — that’s where the future is” to “Good for you! We need more real doctors around here.”
All students with medical aspirations owe it to themselves and their future patients to find their proper niche, where they can utilize their greatest strengths for the benefit of the greatest number.
At the same time, the large assortment of healthcare career paths, acronyms, and job duties can get overwhelming.
To tackle all such paths in one article would be impossible (or at least unreadable), so instead let’s look at one of the most common points of confusion. What are the differences between Nurse Practitioners, Physicians Assistants, and Physicians (both MD and DO)?
Before we begin, it’s important to note that all of the professions I listed above may serve as primary care providers; you can find them writing prescriptions, consulting patients, and otherwise appearing to perform the same tasks and duties. However, this can result in misconceptions. So let’s take a closer look and dissect the differences in role, training, autonomy, and salary.
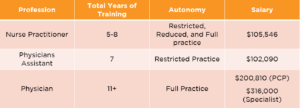
The chart below highlights the total amount of time spent in training, the amount of autonomy allowed in the day-to-day of the job, and the expected salary of each profession.
Nurse Practitioners (NPs)
According to the American Association of Nurse Practitioners (AANP), NPs are “clinicians that blend clinical expertise in diagnosing and treating health conditions with an added emphasis on disease prevention and health management.” Though the requirements for certification differ between states and the type of healthcare setting, all begin their education by obtaining a nursing undergraduate degree (BSN), which involves passing the NCLEX-RN exam and becoming a registered nurse (RN).
Registered nurses can then attend either a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP) program, which generally takes around three years to complete. Many Nurse Practitioners do not directly enter graduate school after undergrad, but instead opt to work as a BSN in order to gain clinical experience, which some graduate programs (but not all) require.
Job Autonomy of a Nurse Practitioner
The autonomy of NPs within their specialty of choice differs by state and tends to be a hot topic for debate within the world of healthcare. Currently, the laws are varied and can be a bit confusing. Though all NPs may prescribe medications, the types of medications (narcotics in particular) differ per local laws. Additionally, some states (known as restrictive) only allow NPs to practice under the supervision of a physician. In other states, NPs are allowed full autonomy, while others have arrangements that fall somewhere in the middle.
“The autonomy of NPs within their specialty of choice differs by state and tends to be a hot topic for debate within the world of healthcare.”
NPs are also specialized, choosing one or more specialties from a set of patient population focus areas. However, the vast majority of NPs (86.6%) are certified in an area of primary care, indicating that this is their primary role within the United States.
Salary of Nurse Practitioners
As far as salary goes, NPs are well paid for their work, averaging $105,546 per year in 2017. The average registered nurse who does not continue on to become a nurse practitioner can expect to make an average salary of $68,450 per year.
Physician Assistants (PAs)
The Physician Assistant is another common mid-level provider. PAs share some marked similarities with NPs, but they differ in many ways as well.
The main role of a PA is to perform examinations, diagnose patients, prescribe treatment plans, provide medical consultation, and otherwise perform many of the same tasks as physicians, while under a physician’s supervision.
According to the American Academy of Physician Assistants, “PAs are certified as medical generalists with a foundation in primary care.” The main role of a PA is to perform examinations, diagnose patients, prescribe treatment plans, provide medical consultation, and otherwise perform many of the same tasks as physicians, while under a physician’s supervision.
How to Become a Physician Assistant
PAs are usually not nurses. Those on the PA track do not attend a nursing undergraduate program, but instead may pursue a variety of majors. In fact, PA programs are more similar to medical school programs in that they require a set of prerequisite courses, including anatomy, physiology, microbiology, general biology, and chemistry. Thus, you will find many pre-PAs majoring in subjects like biology and chemistry.
The hallmark of most PA programs is their clinical hour requirement. Prior to admittance into PA school, students are encouraged to obtain around three years of hands-on experience in a role such as paramedic, technician, or Certified Nursing Assistant (CNA).
Thus, those who attend an undergraduate program as a traditional student must find the time to work hundreds, if not thousands, of clinical hours should they wish to apply directly to a PA program, while simultaneously fulfilling the needs of a demanding major.
The curricula of PA programs are derived from those of medical schools, and it takes about three years to complete the program (including a year of supervised rotations). Once a PA has graduated and passed the relevant national certification exam, he or she is free to practice under the supervision of a physician.
Job Autonomy of a Physician Assistant
Whereas NPs can sometimes practice without the supervision of a consulting physician, Physician Assistants generally work under the guidance of an MD or DO. As with NPs, the states have varying laws regarding the limitations of practice and prescriptions that can be handled by PAs.
In 2016 data found by the Statistical Profile of Certified Physicians Assistants, only 27.8% of PAs were found to work in primary care. The remaining percentage worked within a variety of specialties and subspecialties (including cardiology, gastroenterology, etc.), and surgical specialties.
Salary of a Physician Assistant
PAs are compensated on a similar level as NPs, with a mean 2016 salary of $102,090. While they may be operating in a way that more resembles a physician, their salary tends to be lower because the number of hours worked is usually lower and more regular than those of an MD or DO. PAs can generally decide to work a routine schedule during the week.
“The hallmark of most PA programs is their clinical hour requirement. Prior to admittance into PA school, students are encouraged to obtain around three years of hands-on experience in a role such as paramedic, technician, or Certified Nursing Assistant (CNA).”
Physicians (MDs and DOs)
Physicians are the most intensively trained clinicians, benefiting from a rigorous curriculum designed to produce highly skilled and compassionate healthcare leaders. They are responsible for maintaining the physical and mental health of the populace through the utilization of medically informed diagnoses, evidence-based treatments, cutting-edge technology, patient education, and considerate care. They exist in all manner of specialties and subspecialties across the full spectrum of healthcare.
Prospective medical students must complete the required prerequisites for medical school, which usually include biology, general and organic chemistry, basic physics, English and school-specific recommended or required courses. Many pre-med students major in biology, one of its various biomedical offshoots, chemistry, or the like.
Physicians are the most intensively trained clinicians, benefiting from a rigorous curriculum designed to produce highly skilled and compassionate healthcare leaders.
How to Become a Physician
By junior year, pre-meds take the Medical College Admission Test (MCAT) and apply to medical school. Once accepted, they receive two years of extensive training in advanced courses pertinent to their career (anatomy, pharmacology, human behavior, etc.) and then go on to two years of rotations throughout the many different specialties of medicine.
Job Autonomy of a Physician
After completing their fourth year, medical students become physicians and move on to residency, where they further hone and refine their skills for a minimum of three years before being able to practice on their own. In sum, this entails a minimum of 11 years of training. However, once they are fully trained, they are entirely autonomous in their particular practice. This means that they are directly observing symptoms, weighing the options, choosing a method of treatment, and ordering the execution of the treatment without needing to consult an authority figure. This does not mean that doctors don’t consult with other physicians, nurses, residents, etc., but they are able to act entirely on their own.
Salary of a Physician
The compensation for this intensive track is proportional to the time and effort it demands. In 2017, primary care physicians earned an average salary of $200,810 per year. Specialists, who undergo even more training, averaged a healthy $316,000. This may seem like a huge jump in salary, but it is important to remember how much extra time and money goes into the training necessary to become a specialized physician. Considering the average debt of a newly trained physician, these salaries are often times necessary to pay back their student debt.
Conclusion
No matter the part you play, an effective healthcare system takes a full team of professionals to run efficiently. Although every member is vital, physicians act as the leaders. Contrary to what some may think, this does not imply an elevation of status, but rather a willingness to serve and bear the burden of intense education, long hours, frustrating systems, mountains of paperwork, and great responsibility.
“Ultimately, whether you aspire to be an NP, PA, MD or DO, remember this: whichever healthcare path you choose, your priority must always be to provide the highest level of patient care.”
In recent years, however, NPs and PAs have taken on more autonomy and responsibility as many doctors have moved toward specialties and hospital employment. The trend is multifaceted and may be attributed to a series of interconnected issues including rising medical school tuition (prompting students to seek a higher paying specialty), the primary care provider (PCP) shortage, changes in healthcare culture, faster tracks to practice for PAs and NPs, and of course political influence.
Ultimately, whether you aspire to be an NP, PA, MD or DO, remember this: whichever healthcare path you choose, your priority must always be to provide the highest level of patient care. In what other world do the decisions so often literally mean life or death?